Causes Of Acquired Flat Foot
Overview
The adult acquired flatfoot (AAF) is a progressive, symptomatic (painful) deformity resulting from gradual stretch (attenuation) of the tibialis posterior tendon as well as the ligaments that support the arch of the foot. Although the posterior tibialis tendon plays a significant role, this pathology has recently been recognized as involving failure of other interosseous ligaments, such as the spring ligament. Due to the complexity of this pathology, posterior tibial tendon dysfunction (PTTD) is now referred to as adult acquired flatfoot. Severe flatfoot associated with AAF can lead to other problems, such as plantar fascial tension, tendon pain, rearfoot subluxation, and ankle osteoarthritis. 
Causes
As the name suggests, adult-acquired flatfoot occurs once musculoskeletal maturity is reached, and it can present for a number of reasons, though one stands out among the others. While fractures, dislocations, tendon lacerations, and other such traumatic events do contribute to adult-acquired flatfoot as a significant lower extremity disorder, as mentioned above, damage to the posterior tibial tendon is most often at the heart of adult-acquired flatfoot. One study further elaborates on the matter by concluding that ?60% of patients [presenting with posterior tibial tendon damage and adult-acquired flatfoot] were obese or had diabetes mellitus, hypertension, previous surgery or trauma to the medial foot, or treatment with steroids?.
Symptoms
The types of symptoms that may indicate Adult-Acquired Flat Foot Deformity include foot pain that worsens over time, loss of the arch, abnormal shoe wear (excessive wearing on the inner side of shoe from walking on the inner side of the foot) and an awkward appearance of the foot and ankle (when viewed from behind, heel and toes appear to go out to the side). It is important that we help individuals recognize the early symptoms of this condition, as there are many treatment options, depending upon the severity, the age of the patient, and the desired activity levels.
Diagnosis
Starting from the knee down, check for any bowing of the tibia. A tibial varum will cause increased medial stress on the foot and ankle. This is essential to consider in surgical planning. Check the gastrocnemius muscle and Achilles complex via a straight and bent knee check for equinus. If the range of motion improves to at least neutral with bent knee testing of the Achilles complex, one may consider a gastrocnemius recession. If the Achilles complex is still tight with bent knee testing, an Achilles lengthening may be necessary. Check the posterior tibial muscle along its entire course. Palpate the muscle and observe the tendon for strength with a plantarflexion and inversion stress test. Check the flexor muscles for strength in order to see if an adequate transfer tendon is available. Check the anterior tibial tendon for size and strength.
Non surgical Treatment
Conservative treatment is indicated for nearly all patients initially before surgical management is considered. The key factors in determining appropriate treatment are whether acute inflammation and whether the foot deformity is flexible or fixed. However, the ultimate treatment is often determined by the patients, most of whom are women aged 40 or older. Compliance can be a problem, especially in stages I and II. It helps to emphasise to the patients that tibialis posterior dysfunction is a progressive and chronic condition and that several fittings and a trial of several different orthoses or treatments are often needed before a tolerable treatment is found. 
Surgical Treatment
Types of surgery your orthopaedist may discuss with you include arthrodesis, or welding (fusing) one or more of the bones in the foot/ankle together. Osteotomy, or cutting and reshaping a bone to correct alignment. Excision, or removing a bone or bone spur. Synovectomy, or cleaning the sheath covering a tendon. Tendon transfer, or using a piece of one tendon to lengthen or replace another. Having flat feet is a serious matter. If you are experiencing foot pain and think it may be related to flat feet, talk to your orthopaedist.
Adult Aquired FlatFoot
One in four adults in the U.S. has adult acquired flatfoot deformity, which may begin during childhood or be acquired with age. The foot may be flat all the time or may lose its arch when the person stands. The most common and serious cause of flat foot is Posterior Tibial Tendon Dysfunction, in which the main tendon that supports the arch gradually weakens.
Causes
As discussed above, many health conditions can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to hold up the arch and support your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms here. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
In the early stages of dysfunction of the posterior tibial tendon, most of the discomfort is located medially along the course of the tendon and the patient reports fatigue and aching on the plantar-medial aspect of the foot and ankle. Swelling is common if the dysfunction is associated with tenosynovitis. As dysfunction of the tendon progresses, maximum pain occurs laterally in the sinus tarsi because of impingement of the fibula against the calcaneus. With increasing deformity, patients report that the shape of the foot changes and that it becomes increasingly difficult to wear shoes. Many patients no longer report pain in the medial part of the foot and ankle after a complete rupture of the posterior tibial tendon has occurred; instead, the pain is located laterally. If a fixed deformity has not occurred, the patient may report that standing or walking with the hindfoot slightly inverted alleviates the lateral impingement and relieves the pain in the lateral part of the foot.
Non surgical Treatment
Conservative treatment is indicated for nearly all patients initially before surgical management is considered. The key factors in determining appropriate treatment are whether acute inflammation and whether the foot deformity is flexible or fixed. However, the ultimate treatment is often determined by the patients, most of whom are women aged 40 or older. Compliance can be a problem, especially in stages I and II. It helps to emphasise to the patients that tibialis posterior dysfunction is a progressive and chronic condition and that several fittings and a trial of several different orthoses or treatments are often needed before a tolerable treatment is found.

Surgical Treatment
Surgery is usually performed when non-surgical measures have failed. The goal of surgery is to eliminate pain, stop progression of the deformity and improve a patient?s mobility. More than one technique may be used, and surgery tends to include one or more of the following. The tendon is reconstructed or replaced using another tendon in the foot or ankle The name of the technique depends on the tendon used. Flexor digitorum longus (FDL) transfer. Flexor hallucis longus (FHL) transfer. Tibialis anterior transfer (Cobb procedure). Calcaneal osteotomy - the heel bone may be shifted to bring your heel back under your leg and the position fixed with a screw. Lengthening of the Achilles tendon if it is particularly tight. Repair one of the ligaments under your foot. If you smoke, your surgeon may refuse to operate unless you can refrain from smoking before and during the healing phase of your procedure. Research has proven that smoking delays bone healing significantly.
Achilles Tendonitis Causes And Treatments
 Achilles tendinitis is when the tendon that connects the back of your leg to your heel becomes swollen and painful near the bottom of the foot. This tendon is called the Achilles tendon. It is used for walking, running, and jumping.
Achilles tendinitis is when the tendon that connects the back of your leg to your heel becomes swollen and painful near the bottom of the foot. This tendon is called the Achilles tendon. It is used for walking, running, and jumping.
Causes
Tendinitis can result from an injury or over-use. Improper stretching prior to exertion or incorrect form during physical activity can also contribute to the development of tendinitis. Some people, including those with ?flat feet,? tight tendons or arthritis, are particularly prone to tendinitis.
Symptoms
Pain anywhere along the tendon, but most often on or close to the heel. Swelling of the skin over the tendon, associated with warmth, redness and tenderness. Pain on rising up on the toes and pain with pushing off on the toes. If you are unable to stand on your toes you may have ruptured the tendon. This requires urgent medical attention. A painful heel for the first few minutes of walking after waking up in the morning. Stiffness of the ankle, which often improves with mild activity.
Diagnosis
During an examination of the foot and ankle, you doctor will look for the following signs, Achilles tendon swelling or thickening. Bone spurs appearing at the lower part of the tendon at the back of the hell. Pain at the middle or lower area of the Achilles tendon. Limited range of motion of the foot and ankle, and a decreased ability to flex the foot. Your doctor may perform imaging tests, such as X-rays and MRI scans, to make a diagnosis of Achilles tendinitis. X-rays show images of the bones and can help the physician to determine if the Achilles tendon has become hardened, which indicated insertional Achilles tendinitis. MRI scans may not be necessary, but they are important guides if you are recommended to have surgical treatment. An MRI can show the severity of the damage and determine what kind of procedure would be best to address the condition.
Nonsurgical Treatment
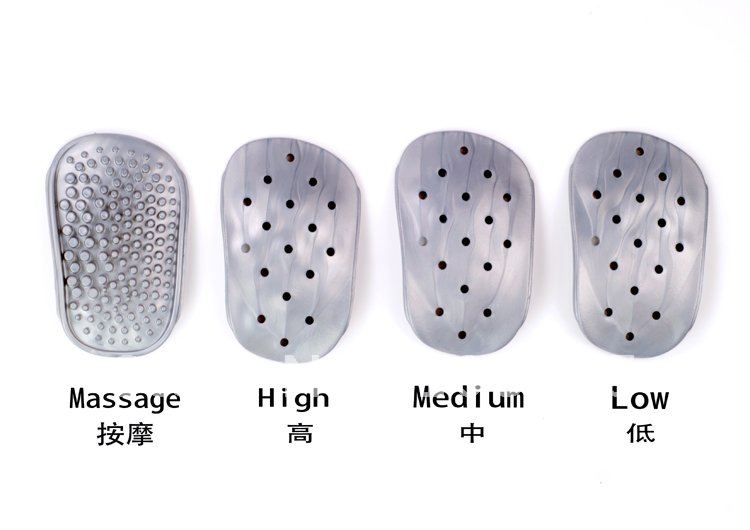
The main treatments for Achilles tendinitis do not involve surgery. It is important to remember that it may take at least 2 to 3 months for the pain to go away. Try putting ice over the Achilles tendon for 15 to 20 minutes, two to three times per day. Remove the ice if the area gets numb. Changes in activity may help manage the symptoms. Decrease or stop any activity that causes you pain. Run or walk on smoother and softer surfaces. Switch to biking, swimming, or other activities that put less stress on the Achilles tendon. Your health care provider or physical therapist can show you stretching exercises for the Achilles tendon. They may also suggest the following changes in your footwear, a brace or boot or cast to keep the heel and tendon still and allow the swelling to go down, heel lifts placed in the shoe under the heel, shoes that are softer in the areas over and under the heel cushion. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen can help with pain or swelling. Talk with your health care provider. If these treatments do not improve symptoms, you may need surgery to remove inflamed tissue and abnormal areas of the tendon. Surgery also can be used to remove the bone spur that is irritating the tendon. Extracorporeal shock wave therapy (ESWT) may be an alternative to surgery for people who have not responded to other treatments. This treatment uses low-dose sound waves.
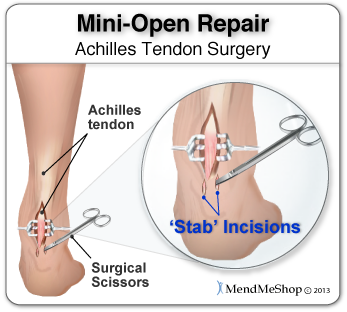
Surgical Treatment
Surgery is considered the last resort. It is only recommended if all other treatment options have failed after at least six months. In this situation, badly damaged portions of the tendon may be removed. If the tendon has ruptured, surgery is necessary to re-attach the tendon. Rehabilitation, including stretching and strength exercises, is started soon after the surgery. In most cases, normal activities can be resumed after about 10 weeks. Return to competitive sport for some people may be delayed for about three to six months.
Prevention
The following measures can significantly reduce the risk of developing Achilles tendonitis. Adequately stretch and warm up prior to exercise. Warm down and stretch after exercise. Choose footwear carefully and use footwear appropriate to the sport being undertaken. Use orthotic devices in footwear to correctly support the foot. Exercise within fitness levels and follow a sensible exercise programme. Develop strong, flexible calf muscles.
Indicators And Treatment For Diabetic Foot


The delayed- or non-healing of wounds is one of the major diabetes complications that cause suffering in people with diabetes and results in more than 500,000 new diabetic foot ulcers and 50,000 lower extremity amputations per year in the US alone. University of Notre Dame researchers have, for the first time, identified the enzymes that are detrimental to diabetic wound healing and those that are beneficial to repair the wound. On the other hand, type 2 diabetes is said to occur in middle-aged and the elderly, who suffer from problems in relation to obesity. Though most women experience these symptoms, in many cases, people suffering from type II diabetes do not experience any symptom for years. Usually, type 2 diabetes is diagnosed after serious health problems, like heart attacks, or vision problems arise. The International Symposium on the Diabetic Foot has become the standard international (scientific) meeting on this topic.
There is in this case, a problem for the diabetic in telling the difference between sharp pain and a more dull pain. Consequently major cuts and wounds often go undetected and diabetic foot ulcers can become problematic. However without effective feedback from the nerves in your foot ot toe, then that adjustment is not adequately made.
Diabetic foot ulcers as one of the most common complications of diabetes mellitus are defined as nonhealing or long-lasting chronic skin ulcers in diabetic patients. Low level laser therapy (LLLT) on wound areas as well as on acupuncture points, as a noninvasive, pain-free method with minor side effects, has been considered as a possible treatment option for the diabetic foot syndrome. The majority of clinical studies show a potential benefit of LLLT in wound healing of diabetic ulcers.
The prevalence of peripheral vascular disease was 15%, hallux vulgus was 22.5%, inappropriate foot wear was 41%, and peripheral neuropathy was 47.5%. Peripheral neuropathy and inappropriate foot wear were the most common risk factors for foot ulceration. Foot ulceration, secondary to diabetes, is the most common reason for lower limb amputation, accounting for 50-70% of non-traumatic lower limb amputations. Rather than progressing through the usual wound healing phases, diabetic wounds become ‘stuck', predominantly in the inflammatory phase. Chronic diabetic wounds always have a bacterial load, and the increased tissue bacterial burden may impede healing. This review seeks to examine factors that prevent diabetic wound healing and the potential of four bee products to promote diabetic human healing in these wounds. Anyone who has diabetes can develop a foot ulcer.
A physical therapist will teach a patient exercises and use specific modalities to help improve symptoms, increase muscle strength and improve control. Therefore, a patient should be Hallux Valgus sure to attend all physical therapy sessions in order to gain the maximum benefit for peripheral neuropathy. Peripheral neuropathy denotes damage to nerve endings in our extremities.
What Exactly Triggers Heel Discomfort
Overview
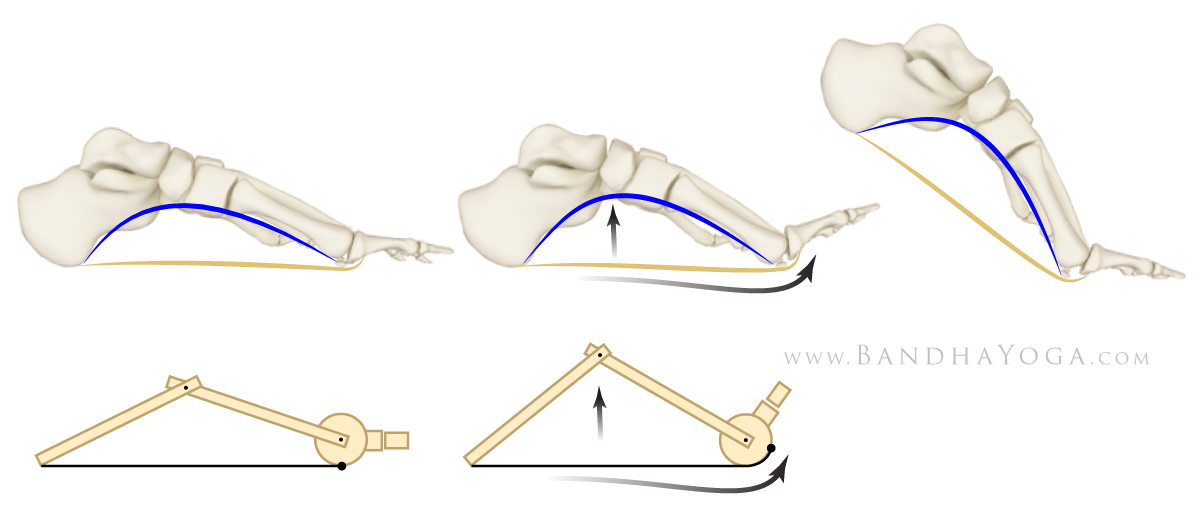
Plantar fasciitis is a condition characterised by damage and inflammation to the plantar fascia (i.e. the connective tissue on the sole of the foot forming the inner arch. This usually occurs at the attachment of the plantar fascia to the heel bone. Plantar fasciitis is the most common cause of heel pain seen in clinical practice. During walking or running, tension is placed through the plantar fascia. When this tension is excessive (often due to poor foot biomechanics such as flat feet or if it is too repetitive or forceful, damage to the plantar fascia can occur. Plantar fasciitis is a condition where there is damage to the plantar fascia with subsequent inflammation and degeneration. This may occur traumatically due to a high force going through the plantar fascia beyond what it can withstand or, more commonly, due to gradual wear and tear associated with overuse. Occasionally, a heel spur may develop in association with plantar fasciitis.
Causes
You are at a greater risk for developing plantar fasciitis if you are overweight or obese. This is due to the increased pressure on your plantar fascia ligaments, especially if you have sudden weight gain. Women who are pregnant often experience bouts of plantar fasciitis, particularly during late pregnancy. If you are a long distance runner, you may be more likely to develop plantar fascia problems. You are also at risk if you have a very active job that involves being on your feet often, such as a factory worker or a restaurant server. Active men and women between the ages of 40 and 70 are at the highest risk for developing plantar fasciitis. It is also slightly more common in women than men. If you have foot problems, such as very high arches or very flat feet, you may develop plantar fasciitis. Tight Achilles tendons (the tendons attaching the calf muscles to the heels) may also result in plantar fascia pain. Simply wearing shoes with soft soles and poor arch support can also result in plantar fasciitis. Plantar fasciitis is not caused by heel spurs. A heel spur is a hook of bone that can form on the heel bone (calcaneus) of the foot. One out of every 10 people has a heel spur, but only one out of 20 people with heel spurs experience pain, according to OrthoInfo.
Symptoms
People with this condition sometimes describe the feeling as a hot, sharp sensation in the heel. You usually notice the pain first thing in the morning when you stand. After walking for a period of time, the pain usually lessens or even disappears. However, sharp pain in the center of the heel may return after resting for a period of time and then resuming activity.
Diagnosis
Your doctor will check your feet and watch you stand and walk. He or she will also ask questions about your past health, including what illnesses or injuries you have had. Your symptoms, such as where the pain is and what time of day your foot hurts most. How active you are and what types of physical activity you do. Your doctor may take an X-ray of your foot if he or she suspects a problem with the bones of your foot, such as a stress fracture.
Non Surgical Treatment
To alleviate the stress and pain on the fascia, the person can take shorter steps and avoid walking barefoot. Activities that involve foot impact, such as jogging, should be avoided. The most effective treatments include the use of in-shoe heel and arch cushioning with calf-stretching exercises and night splints that stretch the calf and plantar fascia while the patient sleeps. Prefabricated or custom-made foot orthotics may also alleviate fascial tension and symptoms. Other treatments may include activity modifications, NSAIDs, weight loss in obese patients, cold and ice massage therapy, and occasional corticosteroid injections. However, because corticosteroid injections can predispose to plantar fasciosis, many clinicians limit these injections. For recalcitrant cases, physical therapy, oral corticosteroids, and cast immobilization should be used before surgical intervention is considered. A newer form of treatment for recalcitrant types of plantar fasciosis is extracorporeal pulse activation therapy (EPAT), in which low-frequency pulse waves are delivered locally using a handheld applicator. The pulsed pressure wave is a safe, noninvasive technique that stimulates metabolism and enhances blood circulation, which helps regenerate damaged tissue and accelerate healing. EPAT is being used at major medical centers.

Surgical Treatment
Surgery should be reserved for patients who have made every effort to fully participate in conservative treatments, but continue to have pain from plantar fasciitis. Patients should fit the following criteria. Symptoms for at least 9 months of treatment. Participation in daily treatments (exercises, stretches, etc.). If you fit these criteria, then surgery may be an option in the treatment of your plantar fasciitis. Unfortunately, surgery for treatment of plantar fasciitis is not as predictable as a surgeon might like. For example, surgeons can reliably predict that patients with severe knee arthritis will do well after knee replacement surgery about 95% of the time. Those are very good results. Unfortunately, the same is not true of patients with plantar fasciitis.
Stretching Exercises
Stretching your plantar fasciitis is something you can do at home to relieve pain and speed healing. Ice massage performed three to four times per day in 15 to 20 minute intervals is also something you can do to reduce inflammation and pain. Placing arch supports in your shoes absorbs shock and takes pressure off the plantar fascia.
What Triggers Plantar Fasciitis To Surface

Overview
Plantar fasciitis is a painful condition causing heel pain and many people with the condition also have heel spurs. It affects the band of tissue (plantar fascia) that supports the middle part of the foot and runs along the sole of the foot from the heel to the ball of the foot. Usually the plantar fascia is strong and flexible but due to certain factors it can become irritated and inflamed where the plantar fascia joins the bone in the foot. Heel spurs occur when there's constant pulling of the fascia at the heel bone. This leads to a bony growth or spur. The symptoms of plantar fasciitis are pain in the arch of the foot or heel. This pain is usually worse in the morning after rest when the plantar fascia tightens and shortens. Heel spurs cause a stabbing pain at the bottom or front of the heel bone.
Causes
Under normal circumstances, your plantar fascia acts like a shock-absorbing bowstring, supporting the arch in your foot. If tension on that bowstring becomes too great, it can create small tears in the fascia. Repetitive stretching and tearing can cause the fascia to become irritated or inflamed.
Symptoms
People with this condition sometimes describe the feeling as a hot, sharp sensation in the heel. You usually notice the pain first thing in the morning when you stand. After walking for a period of time, the pain usually lessens or even disappears. However, sharp pain in the center of the heel may return after resting for a period of time and then resuming activity.
Diagnosis
Your doctor will ask you about the kind of pain you're having, when it occurs and how long you've had it. If you have pain in your heel when you stand up for the first time in the morning, you may have plantar fasciitis. Most people with plantar fasciitis say the pain is like a knife or a pin sticking into the bottom of the foot. After you've been standing for a while, the pain becomes more like a dull ache. If you sit down for any length of time, the sharp pain will come back when you stand up again.
Non Surgical Treatment
Anti-inflammatory agents used in the treatment of plantar fasciitis include ice, NSAIDs, iontophoresis and cortisone injections. Ice is applied in the treatment of plantar fasciitis by ice massage, ice bath or in an ice pack. For ice massage, the patient freezes water in a small paper or foam cup, then rubs the ice over the painful heel using a circular motion and moderate pressure for five to 10 minutes. To use an ice bath, a shallow pan is filled with water and ice, and the heel is allowed to soak for 10 to 15 minutes. Patients should use neoprene toe covers or keep the toes out of the ice water to prevent injuries associated with exposure to the cold. Crushed ice in a plastic bag wrapped in a towel makes the best ice pack, because it can be molded to the foot and increase the contact area. A good alternative is the use of a bag of prepackaged frozen corn wrapped in a towel. Ice packs are usually used for 15 to 20 minutes. Icing is usually done after completing exercise, stretching, strengthening and after a day's work.

Surgical Treatment
Plantar fasciotomy is often considered after conservative treatment has failed to resolve the issue after six months and is viewed as a last resort. Minimally invasive and endoscopic approaches to plantar fasciotomy exist but require a specialist who is familiar with certain equipment. Heel spur removal during plantar fasciotomy has not been found to improve the surgical outcome. Plantar heel pain may occur for multiple reasons and release of the lateral plantar nerve branch may be performed alongside the plantar fasciotomy in select cases. Possible complications of plantar fasciotomy include nerve injury, instability of the medial longitudinal arch of the foot, fracture of the calcaneus, prolonged recovery time, infection, rupture of the plantar fascia, and failure to improve the pain. Coblation (TOPAZ) surgery has recently been proposed as alternative surgical approaches for the treatment of recalcitrant plantar fasciitis.
What Is Painful Heel

Overview
The plantar fascia is a band of connective tissue on the bottom of the foot that helps form the arch of the foot. Acute injury or cumulative trauma to the plantar fascia can be a cause of inflammation and heel pain. This is called plantar fasciitis.
Causes
When the foot moves, the plantar fascia stretches and contracts. Plantar fasciitis is caused by the repetitive overstretching of the plantar fascia. If the tension on the plantar fascia is too great, this overstretching causes small tears in the plantar fascia. This in turn causes the plantar fascia to become inflamed and painful. Factors that contribute to the development of plantar fasciitis include having very high arches or flat feet, gender, while anyone can develop plantar fasciitis, it tends to occur more commonly in women, exercises such as running, walking and dancing, particularly if the calf muscles are tight. Activities or occupations that involve walking or standing for long periods of time, particularly on hard surfaces, wearing high heeled shoes or shoes that do not offer adequate arch support and cushioning, being overweight, additional weight increases the tension on the plantar fascia, poor biomechanics, extra tension is placed on the plantar fascia if weight is not spread evenly when standing, walking or running. Some cases of plantar fasciitis may be linked to underlying diseases that cause arthritis, such as ankylosing spondylitis.
Symptoms
Patients with plantar fasciitis typically experience pain underneath the heel and along the inner sole of the foot. In less severe cases, patients may only experience an ache or stiffness in the plantar fascia or heel that increases with rest (typically at night or first thing in the morning) following activities which place stress on the plantar fascia. These activities typically include standing, walking or running excessively (especially up hills, on uneven surfaces or in poor footwear such as thongs), jumping, hopping and general weight bearing activity. The pain associated with this condition may also warm up with activity in the initial stages of injury. As the condition progresses, patients may experience symptoms that increase during sport or activity, affecting performance. In severe cases, patients may walk with a limp or be unable to weight bear on the affected leg. Patients with this condition may also experience swelling, tenderness on firmly touching the plantar fascia (often on a specific spot on the inner aspect of the heel) and sometimes pain on performing a plantar fascia stretch.
Diagnosis
A health care professional will ask you whether you have the classic symptoms of first-step pain and about your activities, including whether you recently have intensified your training or changed your exercise pattern. Your doctor often can diagnose plantar fasciitis based on your history and symptoms, together with a physical examination. If the diagnosis is in doubt, your doctor may order a foot X-ray, bone scan or nerve conduction studies to rule out another condition, such as a stress fracture or nerve problem.
Non Surgical Treatment
A steroid (cortisone) injection is sometimes tried if your pain remains bad despite the above 'conservative' measures. It may relieve the pain in some people for several weeks but does not always cure the problem. It is not always successful and may be sore to have done. Steroids work by reducing inflammation. Sometimes two or three injections are tried over a period of weeks if the first is not successful. Steroid injections do carry some risks, including (rarely) tearing (rupture) of the plantar fascia. Extracorporeal shock-wave therapy. In extracorporeal shock-wave therapy, a machine is used to deliver high-energy sound waves through your skin to the painful area on your foot. It is not known exactly how it works, but it is thought that it might stimulate healing of your plantar fascia. One or more sessions of treatment may be needed. This procedure appears to be safe but it is uncertain how well it works. This is mostly because of a lack of large, well-designed clinical trials. You should have a full discussion with your doctor about the potential benefits and risks. In studies, most people who have had extracorporeal shock-wave therapy have little in the way of problems. However, possible problems that can occur include pain during treatment, skin reddening, and swelling of your foot or bruising. Another theoretical problem could include the condition getting worse because of rupture of your plantar fascia or damage to the tissues in your foot. More research into extracorporeal shock-wave therapy for plantar fasciitis is needed. Other treatments. Various studies and trials have been carried out looking at other possible treatments for plantar fasciitis. Such treatments include injection with botulinum toxin and treatment of the plantar fascia with radiotherapy. These treatments may not be widely available. Some people benefit from wearing a special splint overnight to keep their Achilles tendon and plantar fascia slightly stretched. The aim is to prevent the plantar fascia from tightening up overnight. In very difficult cases, sometimes a plaster cast or a removable walking brace is put on the lower leg. This provides rest, protection, cushioning and slight stretching of the plantar fascia and Achilles tendon. However, the evidence for the use of splint treatment of plantar fasciitis is limited.

Surgical Treatment
When more-conservative measures aren't working, your doctor might recommend steroid shots. Injecting a type of steroid medication into the tender area can provide temporary pain relief. Multiple injections aren't recommended because they can weaken your plantar fascia and possibly cause it to rupture, as well as shrink the fat pad covering your heel bone. Extracorporeal shock wave therapy. In this procedure, sound waves are directed at the area of heel pain to stimulate healing. It's usually used for chronic plantar fasciitis that hasn't responded to more-conservative treatments. This procedure may cause bruises, swelling, pain, numbness or tingling and has not been shown to be consistently effective. Surgery. Few people need surgery to detach the plantar fascia from the heel bone. It's generally an option only when the pain is severe and all else fails. Side effects include a weakening of the arch in your foot.