Do You Really Understand Heel Soreness?

Heel pain is one of the most common conditions treated by podiatrists. It is often a message from the body that something is in need of medical attention. Pain that occurs right after an injury or early in an illness may play a protective role, often warning us about the damage we have suffered. The greatest incidence of heel pain is seen in middle-aged men and women. It is also seen in those who take part in regular sporting activities and those significantly overweight and on their feet a lot. Heel pain can also occur in children, usually between 8 and 13, as they become increasingly active in sporting activities.
Causes
Heel pain has many causes. Heel pain is generally the result of faulty biomechanics (walking gait abnormalities) that place too much stress on the heel bone and the soft tissues that attach to it. The stress may also result from injury, or a bruise incurred while walking, running, or jumping on hard surfaces; wearing poorly constructed footwear (such as flimsy flip-flops); or being overweight.
Symptoms
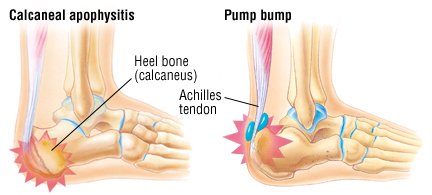
Both heel pain and heel spurs are frequently associated with an inflammation of the long band of tissue that connects the heel and the ball of the foot. The inflammation of this arch area is called plantar fasciitis. The inflammation maybe aggravated by shoes that lack appropriate support and by the chronic irritation that sometimes accompanies an athletic lifestyle. Achilles Tendinopathy, Pain and inflammation of the tendon at the back of the heel that connects the calf muscle to the foot. Sever?s, Often found in children between the ages of 8 - 13 years and is an inflammation of the calcaneal epiphyseal plate (growth plate) in the back of the heel. Bursitis, An inflamed bursa is a small irritated sack of fluid at the back of the heel. Other types of heel pain include soft tissue growths, Haglunds deformity (bone enlargement at the back of the heel), bruises or stress fractures and possible nerve entrapment.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
Most patients get better with the help of nonsurgical treatments. Stretches for the calf muscles on the back of the lower leg take tension off the plantar fascia. A night splint can be worn while you sleep. The night splint keeps your foot from bending downward. It places a mild stretch on the calf muscles and the plantar fascia. Some people seem to get better faster when using a night splint. They report having less heel pain when placing the sore foot on the ground in the morning. There have been a few studies that reported no significant benefit from adding night splinting to a program of antiinflammatory meds and stretching. Other studies report the benefits of short-term casting to unload the heel, immobilize the plantar fascia, and reduce repetitive microtrauma. Supporting the arch with a well fitted arch support, or orthotic, may also help reduce pressure on the plantar fascia. Placing a special type of insert into the shoe, called a heel cup, can reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration. Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Surgical Treatment
When a diagnosis of plantar fasciitis is made early, most patients respond to conservative treatment and don?t require surgical intervention. Often, when there is a secondary diagnosis contributing to your pain, such as an entrapped nerve, and you are non-responsive to conservative care, surgery may be considered. Dr. Talarico will discuss all options and which approach would be the most beneficial for your condition.
How do you treat heel pain?
Prevention
Being overweight can place excess pressure and strain on your feet, particularly on your heels. Losing weight, and maintaining a healthy weight by combining regular exercise with a healthy, balanced diet, can be beneficial for your feet. Wearing appropriate footwear is also important. Ideally, you should wear shoes with a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels.
Guidelines On How To Combat Pes Planus

Fairly common in infants and small children, but also prevalent in adults, flat feet becomes a problem if pain or discomfort is present in the foot or even around the knee and lower leg area. Pain around the knee and lower leg areas can arise because flat feet can alter proper foot and leg alignment, which will put unusual strain on the knee. Adults can develop the condition as the result of injury or even from normal wear and tear due to the natural aging process.
Causes
There are a number of different causes that can lead to flat feet or fallen arches. These include, birth defects, while technically not a defect as such, flat feet can be a normal finding in patients from birth. However, a condition called tarsal coalition may occur where some of the bones in the foot are fused together resulting in a flatfoot. Inflammation or damage of the posterior tibial tendon. This tendon forms the end of a muscle that connects the lower leg to the foot, winding around the ankle and attaching to the inner aspect where the arch is normally present. The main role of the posterior tibial tendon is to invert the foot and maintain the arch height throughout the gait cycle. Torn muscles of the leg and foot can cause flat feet. Problems with the nerve supply to the muscles can result in reduction in tone and fallen arches. Fracture dislocation of the bones in the foot. Severe arthritis. While these are the common causes that can result in fallen arches and flat feet, it is important to recognise that there are certain risk factors that can also lead to this condition. These include advancing age, diabetes mellitus, high blood pressure, obesity and pregnancy.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
Your doctor examines your feet to determine two things, whether you have flat feet and the cause or causes. An exam may include the following steps, Checking your health history for evidence of illnesses or injuries that could be linked to flat feet or fallen arches, Looking at the soles of your shoes for unusual wear patterns, Observing the feet and legs as you stand and do simple movements, such as raising up on your toes, Testing the strength of muscles and tendons, including other tendons in the feet and legs, such as the Achilles tendon or the posterior tibial tendon, Taking X-rays or an MRI of your feet.
pes planus radiology
Non Surgical Treatment
Most flexible flat feet are asymptomatic, and do not cause pain. In these cases, there is usually no cause for concern, and the condition may be considered a normal human variant. Flat feet were formerly a physical-health reason for service-rejection in many militaries. However, three military studies on asymptomatic adults (see section below), suggest that persons with asymptomatic flat feet are at least as tolerant of foot stress as the population with various grades of arch. Asymptomatic flat feet are no longer a service disqualification in the U.S. military.
Surgical Treatment

Common indications for surgery are cerebral palsy with an equinovalgus foot, to prevent progression and breakdown of the midfoot. Rigid and painful Pes Planus. To prevent progression, eg with a Charcot joint. Tibialis posterior dysfunction, where non-surgical treatment is unsuccessful. Possible surgical procedures include Achilles tendon lengthening. Calcaneal osteotomy, to re-align the hindfoot. Reconstruction of the tibialis posterior tendon. For severe midfoot collapse of the arch, triple arthrodesis may be indicated.
Leg Length Discrepancy After Knee Replacement Surgery
Surgeries for LLD are designed to do one of three general things ? shorten the long leg, stop or slow the growth of the longer or more rapidly growing leg, or lengthen the short leg. Stopping the growth of the longer leg is the most commonly utilized of the three approaches and involves an operation known as an epiphysiodesis , in which the growth plate of either the lower femur or upper tibia is visualized in the operating room using fluoroscopy (a type of real-time radiographic imaging) and ablated , which involves drilling into the region several times, such that the tissue is no longer capable of bone growth. Because the epiphyseal growth capabilities cannot be restored following the surgery, proper timing is crucial. Usually the operation is planned for the last 2 to 3 years of growth and has excellent results, with children leaving the hospital within a few days with good mobility. However, it is only appropriate for LLD of under 5cm.

Causes
Leg discrepancy can develop from a medical issue in any portion of the femur or tibia. One leg may lengthen, but leg shortening is much more common. Factors that can cause leg length discrepancy include inherited growth deficiencies. Infections. A bone infection can cause delayed growth in the affected limb. Injury. If your child breaks a leg, it may be shorter once it heals. This is most likely to happen if the fracture or break was complicated, an open fracture, or an injury that affected the growth plate near the end of the bone. Alternatively, a break can cause bones to grow faster after healing, making a leg longer. Tumors. Legg-Calve-Perthes disease. This is a condition that affects the ball (femoral head) of the hip joint. The femoral head may be friable and damage easily, sometimes leading to shortening of the thigh bone. Hemihypertrophy. In children with this condition, one side of the body grows more quickly than the other. Vascular malformations. These are abnormal clusters of veins and arteries that can form close to the bone and stimulate growth. Juvenile arthritis. Inflammation from arthritis can stimulate growth in the affected leg and cause discrepancy.
Symptoms
Back pain along with pain in the foot, knee, leg and hip on one side of the body are the main complaints. There may also be limping or head bop down on the short side or uneven arm swinging. The knee bend, hip or shoulder may be down on one side, and there may be uneven wear to the soles of shoes (usually more on the longer side).
Diagnosis
Leg length discrepancy may be diagnosed during infancy or later in childhood, depending on the cause. Conditions such as hemihypertrophy or hemiatrophy are often diagnosed following standard newborn or infant examinations by a pediatrician, or anatomical asymmetries may be noticed by a child's parents. For young children with hemihypertophy as the cause of their LLD, it is important that they receive an abdominal ultrasound of the kidneys to insure that Wilm's tumor, which can lead to hypertrophy in the leg on the same side, is not present. In older children, LLD is frequently first suspected due to the emergence of a progressive limp, warranting a referral to a pediatric orthopaedic surgeon. The standard workup for LLD is a thorough physical examination, including a series of measurements of the different portions of the lower extremities with the child in various positions, such as sitting and standing. The orthopaedic surgeon will observe the child while walking and performing other simple movements or tasks, such as stepping onto a block. In addition, a number of x-rays of the legs will be taken, so as to make a definitive diagnosis and to assist with identification of the possible etiology (cause) of LLD. Orthopaedic surgeons will compare x-rays of the two legs to the child's age, so as to assess his/her skeletal age and to obtain a baseline for the possibility of excessive growth rate as a cause. A growth chart, which compares leg length to skeletal age, is a simple but essential tool used over time to track the progress of the condition, both before and after treatment. Occasionally, a CT scan or MRI is required to further investigate suspected causes or to get more sophisticated radiological pictures of bone or soft tissue.
Non Surgical Treatment
The treatment of LLD depends primarily on the diagnosed cause, the age of the patient, and the severity of the discrepancy. Non-operative treatment is usually the first step in management and, in many cases, LLD is mild or is predicted to lessen in the future, based on growth rate estimates in the two legs. In such cases, no treatment may be necessary or can be delayed until a later stage of physical maturity that allows for clearer prognostic approximation. For LLD of 2cm to 2.5cm, treatment may be as simple as insertion of a heel lift or other shoe insert that evens out leg lengths, so to speak. For more severe cases, heel lifts can affect patient comfort when walking, decrease ankle stability, and greatly increase the risk of sprains. For infants with congenital shortening of the limb, a prosthetic ? often a custom-fit splint made of polypropylene ? may be successful in treating more severe LLD without surgery. In many instances, however, a surgical operation is the best treatment for LLD.

how do you get taller in a day?
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
What Causes Mortons Neuroma
 Morton?s neuroma is inflammation, thickening, or enlargement of the nerve between the bones of the toes (metatarsal bones). The condition is also called intermetatarsal neuroma. The thickening is usually found between bones of the third and fourth toes of the foot, but sometimes it may develop between the second and third toes. It occurs when the medial plantar nerve near the bones of those toes becomes compressed or irritated, possibly because the metatarsal bones press against the nerve in the narrow gap between the toes. If left untreated, Morton?s neuroma can cause a sharp, burning, or shooting pain that often gets worse over time. The pain becomes worse when a person walks or stands on the ball of the foot. Sometimes the pain reaches the toes next to the neuroma and a sensation of tingling or numbness is felt.
Morton?s neuroma is inflammation, thickening, or enlargement of the nerve between the bones of the toes (metatarsal bones). The condition is also called intermetatarsal neuroma. The thickening is usually found between bones of the third and fourth toes of the foot, but sometimes it may develop between the second and third toes. It occurs when the medial plantar nerve near the bones of those toes becomes compressed or irritated, possibly because the metatarsal bones press against the nerve in the narrow gap between the toes. If left untreated, Morton?s neuroma can cause a sharp, burning, or shooting pain that often gets worse over time. The pain becomes worse when a person walks or stands on the ball of the foot. Sometimes the pain reaches the toes next to the neuroma and a sensation of tingling or numbness is felt.Causes
Morton's neuroma is an inflammation caused by a buildup of fibrous tissue on the outer coating of nerves. This fibrous buildup is a reaction to the irritation resulting from nearby bones and ligaments rubbing against the nerves. Irritation can be caused by wearing shoes that are too tight, wearing shoes that place the foot in an awkward position, such as high heels, a foot that is mechanically unstable, repetitive trauma to the foot such as from sports activities like tennis, basketball, and running. Trauma to the foot caused by an injury such as a sprain or fracture. It is unusual for more than one Morton's neuroma to occur on one foot at the same time. It is rare for Morton's neuroma to occur on both feet at the same time.
Symptoms
The symptoms of a Morton's neuroma are classic in nature. The patient complains of a burning , tingling, slightly numb feeling (dysesthesias) which radiates out to the toes on either side of the interspace that is involved. For instance, a Morton's neuroma of the third interspace will result in pain between the third and fourth toes, and a neuroma in the second interspace will cause pain between the second and third toes. The symptoms are usually aggravated by wearing shoes, particularly those with high heels. Symptoms are relieved by walking in flat, wide shoes or going barefoot. Rarely will the patient experience pain when sitting or laying down.
Diagnosis
X-rays of your affected foot will not show a neuroma, as neuromas are made up of soft tissue. X-rays may be helpful, however, in helping rule in osteoarthritis or a stress fracture as the cause of your symptoms. Ultrasonography and MRI are sometimes used to help diagnose neuromas, although they are often ineffective. The clinical diagnosis by a foot care expert with experience treating this health problem is usually the most effective way to diagnose neuromas. Your podiatrist will attempt to duplicate your neuroma symptoms by pressing on the involved nerve at various points, and he or she may try to cause a clicking of your nerve that indicates nerve enlargement.
Non Surgical Treatment
Most non-operative treatment is usually successful, although it can take a while to figure out what combination of non-operative treatment works best for each individual patient. Non-operative treatment may include the use of comfort shoe wear. The use of a metatarsal pad to decrease the load through the involved area of the plantar forefoot. A period of activity modification to decrease or eliminate activities, which may be exacerbating the patient?s symptoms. For example, avoiding long periods of standing or other activities that result in significant repetitive loading to the forefoot can be very helpful. Wearing high heels should be avoided. Local can help decrease inflammation associated with the nerve. However, this does not necessarily address the underlying loading forces that maybe causing the injury to the nerve in the first place. It has been proposed that an alcohol injection in and around the nerve will cause a controlled death to the nerve and subsequently eliminate symptoms. In theory, this may be helpful. In practice, adequate prospective studies have not demonstrated the benefit of this procedure above and beyond the other standard, non-operative treatments available. In addition there is the concern that the alcohol will cause excessive scarring and damage to other important structures in the area.

Surgical Treatment
The ultimate success of a Morton?s neuroma treated surgically can be variable. In cases where the underlying problem is only an irritated nerve (a true Morton?s neuroma), then surgery will probably be curative (although it may take a few months for the foot to fully heal). But in many cases, forefoot pain is more complex. There may be an irritated nerve or two causing pain, but the real problem is often excessive loading of the lesser metatarsals. The generic term for this condition is metatarsalgia. When considering surgery, identifying and addressing these problems may lead to a better end result.
Prevention
Wearing shoes that fit properly and that have plenty of room in the toe area may help prevent Morton's neuroma.
Hammer Toe Pain Symptoms
Overview
Hammer toes is a Z-shaped deformity caused by dorsal subluxation at the metatarsophalangeal joint. Diagnosis is clinical. Treatment is modification of footwear and/or orthotics. The usual cause is misalignment of the joint surfaces due to a genetic predisposition toward aberrant foot biomechanics and tendon contractures. RA and neurologic disorders such as Charcot-Marie-Tooth disease are other causes.
Causes
Ill-fitting shoes or a muscle imbalance are the most common causes of Hammer Toe. If there is an issue with a muscle in the second, third or fourth toes preventing them from straightening, Hammer Toe can result. If one of these toes is bent long enough in one position, the muscles tighten and cannot stretch out. Left untreated, surgery may be required. Women are especially prone to developing Hammer Toe because of their shoes. Hammer Toe results from shoes that don?t fit properly. Shoes that narrow toward the toe, pushing smaller toes into a bend position for extended periods of time. High heels that force the foot down into a narrow space, forcing the toes against the shoe, increasing the bend in the toe. .jpg)
Symptoms
Signs and symptoms of hammertoe and mallet toe may include a hammer-like or claw-like appearance of a toe. In mallet toe, a deformity at the end of the toe, giving the toe a mallet-like appearance. Pain and difficulty moving the toe. Corns and calluses resulting from the toe rubbing against the inside of your footwear. Both hammertoe and mallet toe can cause pain with walking and other foot movements.
Diagnosis
First push up on the bottom of the metatarsal head associated with the affected toe and see if the toe straightens out. If it does, then an orthotic could correct the problem, usually with a metatarsal pad. If the toe does not straighten out when the metatarsal head is pushed up, then that indicates that contracture in the capsule and ligaments (capsule contracts because the joint was in the wrong position for too long) of the MTP joint has set in and surgery is required. Orthotics are generally required post-surgically.
Non Surgical Treatment
Any forefoot problems that cause pain or discomfort should be given prompt attention. Ignoring the symptoms can aggravate the condition and lead to a breakdown of tissue, or possibly even infection. Conservative treatment of mallet toes begins with accommodating the deformity. The goal is to relieve pressure, reduce friction, and transfer forces from the sensitive areas. Shoes with a high and broad toe box (toe area) are recommended for people suffering from forefoot deformities such as mallet toes. This prevents further irritation in the toe area from developing. Other conservative treatment includes forefoot supports such as gel toe caps, gel toe shields and toe crests. Gel forefoot supports provide immediate comfort and relief from common forefoot disorders without drying the skin.
Surgical Treatment
For the surgical correction of a rigid hammertoe, the surgical procedure consists of removing the damaged skin where the corn is located. Then a small section of bone is removed at the level of the rigid joint. The sutures remain in place for approximately ten days. During this period of time it is important to keep the area dry. Most surgeons prefer to leave the bandage in place until the patient's follow-up visit, so there is no need for the patient to change the bandages at home. The patient is returned to a stiff-soled walking shoe in about two weeks. It is important to try and stay off the foot as much as possible during this time. Excessive swelling of the toe is the most common patient complaint. In severe cases of hammertoe deformity a pin may be required to hold the toe in place and the surgeon may elect to fuse the bones in the toe. This requires several weeks of recovery. 
Prevention
Preventing foot problems, including hammertoes, is often a matter of wearing the right shoes and taking care of your feet. Check your feet regularly for problems. This is especially true if you have diabetes or any other medical condition that causes poor circulation or numbness in your toes. If you do, check feet daily so that problems can be caught early on.
Flexible Hammertoes Treatment
 Overview
Overview
The 2nd toe is the most common digit to develop a hammertoe deformity. Second toe hammer toes commonly result from an elongated 2nd metatarsal and from pressure due to an excessively abducted great toe (hallux valgus deformity) causing a bunion. Unusually long toes often develop hammer toe deformities. Painful corns often develop in hammer toe deformity, particularly of the 5th toe. Reactive adventitial bursas often develop beneath corns, which may become inflamed.
Causes
Hammer toe is most often caused by wearing compressive shoes. It might also be caused by the pressure from a bunion. A bunion is a corn on the top of a toe and a callus on the sole of the foot develop which makes walking painful. A high foot arch may also develop.
 Symptoms
Symptoms
A hammertoe may be present but not always painful unless irritated by shoes. One may have enlarged toe joints with some thickened skin and no redness or swelling. However, if shoes create pressure on the joint, the pain will usually range from pinching and squeezing to sharp and burning. In long standing conditions, the dislocated joints can cause the pain of arthritis.
Diagnosis
The exam may reveal a toe in which the near bone of the toe (proximal phalanx) is angled upward and the middle bone of the toe points in the opposite direction (plantar flexed). Toes may appear crooked or rotated. The involved joint may be painful when moved, or stiff. There may be areas of thickened skin (corns or calluses) on top of or between the toes, a callus may also be observed at the tip of the affected toe beneath the toenail. An attempt to passively correct the deformity will help elucidate the best treatment option as the examiner determines whether the toe is still flexible or not. It is advisable to assess palpable pulses, since their presence is associated with a good prognosis for healing after surgery. X-rays will demonstrate the contractures of the involved joints, as well as possible arthritic changes and bone enlargements (exostoses, spurs). X-rays of the involved foot are usually performed in a weight-bearing position.
Non Surgical Hammer toe Treatment
Treatment for a hammertoe usually depends on the stage of the hammertoe and the cause of the condition. If your toe is still bendable, your doctor may suggest conservative care-relieving pressure with padding and strapping, or proper shoes that have a deep toe box and are of adequate length and width. Early intervention can often prevent the need for surgery.
Surgical Treatment
Ordinary hammertoe procedures often use exposed wires which extend outside the end of toes for 4-6 weeks. Common problems associated with wires include infection where the wires come out of the toe, breakage, pain from hitting the wire, and lack of rotational stability causing the toe to look crooked. In addition, wires require a second in-office procedure to remove them, which can cause a lot of anxiety for many patients. Once inserted, implants remain within the bone, correcting the pain and deformity of hammertoes while eliminating many of the complications specific traditional treatments.
How To Prevent Bunions From Coming Back
Overview
 A foot bunion is when the big toe gradually deviates inwards towards the second toe and in severe cases may even start to cross over the top or underneath. As the top of the toe moves inwards, the base of the toe (the knuckle part), pushes outwards producing the characteristic lump on outer side of the big toe. The medical term for a foot bunion at the big toe is a hallux abducto valgus, or hallux valgus. ?Hallux? means big toe, ?abducto? means to move away from the midline and ?valgus? refers to the abnormal angle of the toe. Foot bunions can also occur in the little toe, where they are known as a bunionette, but these are much less common.
A foot bunion is when the big toe gradually deviates inwards towards the second toe and in severe cases may even start to cross over the top or underneath. As the top of the toe moves inwards, the base of the toe (the knuckle part), pushes outwards producing the characteristic lump on outer side of the big toe. The medical term for a foot bunion at the big toe is a hallux abducto valgus, or hallux valgus. ?Hallux? means big toe, ?abducto? means to move away from the midline and ?valgus? refers to the abnormal angle of the toe. Foot bunions can also occur in the little toe, where they are known as a bunionette, but these are much less common.
Causes
It is thought that the primary cause of bunions is a mechanical instability in the big toe joint. There are a number of different reasons as to why this may happen. Bunions tend to run in families so a person with a family history of bunions has an increased risk of developing them. Factors that are known to increase the risk of bunions include wearing improperly fitting shoes (particularly narrow and/or high-heeled shoes). Certain arthritic conditions and ligament disorders. Age (the incidence of bunions increases with age). Being flatfooted with feet that roll inwards (over pronation). Past injury (trauma) to the foot. Nerve conditions affecting the foot. Bunions most commonly affect women (approximately 90% of cases) and are less common in people who do not regularly wear shoes.
Symptoms
symptoms and problems caused by bunions include pain. You may then have difficulty walking due to pain. Inflammation and swelling at the base of the toe. This sometimes becomes infected. The foot may become so wide that it can be difficult to find wide enough shoes. You may get arthritis in the big toe. The second toe can become deformed. In severe cases, the big toe can push your second toe up out of place.
Diagnosis
Your doctor will ask questions about your past health and carefully examine your toe and joint. Some of the questions might be: When did the bunions start? What activities or shoes make your bunions worse? Do any other joints hurt? The doctor will examine your toe and joint and check their range of motion. This is done while you are sitting and while you are standing so that the doctor can see the toe and joint at rest and while bearing weight. X-rays are often used to check for bone problems or to rule out other causes of pain and swelling. Other tests, such as blood tests or arthrocentesis (removal of fluid from a joint for testing), are sometimes done to check for other problems that can cause joint pain and swelling. These problems might include gout , rheumatoid arthritis , or joint infection.
Non Surgical Treatment
Most of the time, non-surgical (conservative) treatment can control the symptoms of a foot bunion or bunionette. These include. Appropriate Footwear, changing to wide fitting footwear reduces the pressure on the big toe and prevents shoes from rubbing on the bony lump. When possible, go barefoot Toe stretchers are a really simple way to reduce foot bunion pain. Toe Stretchers, wearing toe spaces that fit in-between the toes help to stretch the muscles and ligaments around the toes, improving the alignment and relieving pain. Find out more about how these work in the Toe Stretcher section. Painkillers, your doctor may prescribe or recommend over-the-counter medication to reduce the pain and inflammation. Foot bunion correctors can be worn in your shoe to help realign your foot if you suffer from foot bunions. Orthotics. There are a number of over-the-counter shoe inserts that can help relieve symptoms. Bunion correctors work by realigning the bones in your foot to reduce pressure on the affected toe. There are both day-time and night-time splints on the market, although the evidence of their effectiveness is lacking. Ice. Applying ice packs to the foot can help reduce pain and inflammation. Bunion pads help to reduce any friction on your big toe. Bunion Pads. You can also get protective foot cushions that sit over the skin to prevent the hallux abducto valgus rubbing on your shoes. 
Surgical Treatment
Bunion surgery is both an art and a science, and it should always be performed by a healthcare professional who understands the multifaceted mechanics of your first MTP and its surrounding structures. Bunion surgery involves more than just removing the bump at the base of your big toe, and it is best followed up with supportive therapies to prevent a recurrence of your health problem.